‘WHAT PROBING DEEP HAS EVER SOLVED THE MYSTERY OF SLEEP?’ - Thomas Bailey Aldrich
Sleep patterns vary from one individual to another, some need only 4-5 hours and others may need 10-12, but in general, adults sleep for about 7-8 hours per night. It is estimated that we spend around one third of our lives asleep and our day-to-day well-being is often measured by our perceived sleep quality. Approximately 35% of the population suffers from insomnia but only about 5% of them consultant their GP12,16.
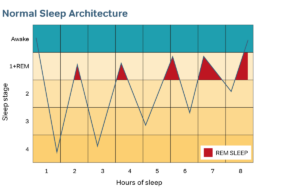
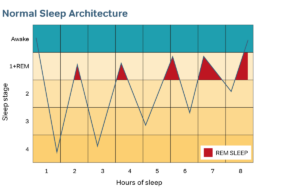
Sleep is divided into two distinct states — Rapid Eye Movement (REM) sleep and non-REM which is further divided into 4 stages: Stage 1 (drowsiness), Stage 2 (light sleep), and Stages 3 & 4 (deep sleep). Deep sleep is often referred to as slow-wave sleep (SWS). These stages of sleep alternate in 70 – 90 minute cycles and in an average night, sleep will move through 4 to 5 cycles. See Figure 1.
However, many individuals rarely obtain a good night’s sleep. Sleep disturbances can be classified according their duration as either transient (<1 week), short-term (1-3 weeks) or chronic (months).
Additionally, they can be a primary disorder or occur secondary to other disorders. Here we will briefly examine the sleep disturbances caused by a range of prescription and over-the-counter (OTCs) medications and also discuss how some lifestyle choices can have a detrimental effect on our sleep.
'PAIN IS THE ROOT OF KNOWLEDGE' - Simone Weil
Pain is probably the most frequent and disabling symptom in medicine. It causes sleep deprivation which can further worsen the severity of the pain. Studies have reported greater sleep disturbance among patients with acute or severe pain and can predict the level of sleep disturbance to the severity of pain11.
Analgesics used in the symptomatic treatment of pain can be broadly divided into 3 categories:
opioids, nonopioids and adjuvant analgesics14.
Opioids include heroin, morphine, methadone and codeine. They are used as major analgesics
and are known for their sedating effects but they also have a profound effect on sleep disturbance. Known disturbances include prolonged sleep latency (SL), decreased SWS and REM, and an increase in arousals throughout the night. Opioids are also known to depress respiratory drive by decreasing the respiratory centre’s sensitivity to carbon dioxide3,14. Kosinski in his study, evaluated the changes in pain and pain-related sleep disturbance with the use of Tramadol. Paradoxically, despite somnolence and insomnia being the most commonly cited adverse events, patients reported significant improvement in their pain-related sleep disturbance11.
Nonopioid analgesics are generally known as nonsteroidal anti-inflammatory drugs (NSAIDs) that include paracetamol, aspirin and ibuprofen. In a study by Onen, paracetamol had a beneficial effect on sleep quality even in patients free of pain, whereas aspirin and ibuprofen had a negative effect (increased SL, increased awakenings, decreased SWS). However, Genco in his study, treated healthy subjects with 400mg ibuprofen TID for 3 days, and reported no interference in sleep patterns.
Adjuvant analgesics comprise those drugs that have a primary indication other than pain but are also known to be analgesic in some circumstances. These analgesics usually include antidepressants and anticonvulsants. Although antidepressants supress REM sleep, induce more restless sleep, and sometimes worsen insomnia, according to Lam12 they objectively and subjectively improve quality of sleep in depressed individuals.
‘PEOPLE WHO SAY THEY SLEEP LIKE A BABY USUALLY DON’T HAVE ONE’ - Leo Burke
Benzodiazepines,are among the most commonly prescribed hypnotics. As well as affecting sleep architecture they can have an adverse effect on breathing during sleep. These medications are mild respiratory depressants and can increase the apnoea/hypopnoea index and decrease oxygen saturation. Brown’s study found the mean number of apnoeas increased from 5/hr on a control night to 10/hr on the drug night with oxygen desaturation. This effect is more pronounced in those individuals who suffer from sleep disordered breathing (SDB).
Antidepressants are prescribed for mood disorders but they are sometimes prescribed for use as hypnotics. In polysomnography (PSG) studies antidepressants were found to suppress REM sleep, increase awakenings and arousals and reduce total sleep time (TST)6. There is also the tendency to exacerbate periodic limb movements during sleep and restless leg syndrome3.
Symptoms of sleep abnormalities have been reported to occur in around 60-80% of depressed patients but there have been mixed reports on the use of antidepressants. In one study, improvements in both SL and TST were demonstrated6. However, in Wilson’s study, only an increase in REM onset latency was reported17.
‘PEOPLE WHO SNORE ALWAYS FALL ASLEEP FIRST’ - unknown author
The use of medications for the treatment of sleep-disordered breathing is theoretically attractive. Compared with current treatments (Mandibular Advancement Therapy, CPAP), compliance would improve dramatically if patients simply had to take a daily pill. The use of ventilatory drive stimulants, central nervous system stimulants, antidepressants, serotonin reuptake inhibitors or antagonists, antihypertensive agents and even sedative hypnotics agents have been studied but no data has demonstrated that pharmacologic agents improve upper airway muscle activity9.
Indeed studies have shown that sedatives have a deleterious effect on respiration during sleep, reduced genioglossal muscle tone — with consequent worsening of Obstructive Sleep Apnoea (OSA), increased apnoeas and increase in severity of nocturnal oxygen desaturation9,13. Lu in his study, found some of the physicians (who did not usually treat patients with sleep disorders) prescribed sedatives to patients with undiagnosed OSA who presented with sleep-related symptoms. Of the 50 physicians in the study, only one-third of them screened their patients for OSA prior to prescribing sedatives.
THE BIG 3 - CHALLENGES OF MODERN LIFE
Caffeine is without question the most commonly used stimulant worldwide, with an estimated mean consumption of 210-238mg per person per day3,7. PSG studies demonstrate the most prominent effects of caffeine to be prolonged SL, reduced sleep efficiency, reduced SWS and increased awakenings during sleep.
Alcohol is the second most commonly used psychoactive substance used worldwide3. An estimated 13% of people use alcohol as an aid to sleep. It is similar to sedative hypnotics and has significant effects on sleep. One study reported alcohol users to suffer decreased SL, suppressed REM sleep (dose-dependent) and increased excessive daytime sleepiness, significantly more than nonusers. The authors concluded that continued use of alcohol as a sleep aid exacerbates these disturbances10. The effect of alcohol in alcoholics is different. SL and TST is decreased and their sleep is composed primarily of non-REM sleep. Even after more than 2 years of abstinence, recovering alcoholics show abnormal sleep patterns. Alcohol decreases muscle tone, particularly in the upper airway and leads to the development or worsening of snoring and OSA. It decreases the arousal response so that obstructive events become longer in duration.
Nicotine affects sleep both during use and on withdrawal. PSG studies show that compared to nonsmokers, current smokers experience increased SL, less TST and lower sleep efficiency. Additionally, a drop in nicotine levels in the brain during sleep causes nicotine craving19. This state of withdrawal modifies sleep continuity and subjective results showed smokers experience more difficulties with morning wakefulness and EDS than non-smokers. Cessation of smoking can reverse these conditions.
‘HE SLEEPS WELL WHO IS NOT CONSCIOUS THAT HE SLEEPS ILL’ - Francis Bacon
Insomnia (specifically increased SL) is a common complaint of persons using illicit drugs, although withdrawal from the drug itself can also induce a variety of sleep problems. Increased TST and REM sleep occur during initial abstinence followed by persistent insomnia and REM disturbance for several weeks after. For some, sleep disturbance is so severe it can inhibit treatment success with consequent relapse to addiction3,15.
In asthma and allergic rhinitis inflammation increases at night often leading to disturbed sleep. The use of antihistamines and decongestants is common but the side effects of these medications can cause insomnia and subsequent daytime fatigue18.
Patients with Alzheimer’s disease (AD) commonly have poor sleep and a high incidence of SDB. Sleep disturbance in AD may be multifactorial and involve SDB and disrupted chronobiology often characterised by excessive daytime napping1. In a study by Cooke4, PSG results demonstrated that AD patients with SDB spent less of the night in REM sleep than those with no SDB, but there were no differences in other sleep stages. In a further study by Cooke5, it was found that Acetylcholinesterase Inhibitors (AChEls) used in AD, changed sleep architecture significantly. There were changes to stages 1 & 2 sleep, but no changes to REM or SWS. A better understanding of the cause-and-effect relationship of AChEls is needed to further understand their effects on sleep architecture. Meanwhile treating these patients’ SDB may improve their daytime functioning.
‘SLEEP IS THE GOLDEN CHAIN THAT TIES OUR HEALTH AND BODIES TOGETHER’ - Thomas Dekker
Although the effects of a drug are known, some medications may act differently in individuals who are more susceptible to sleep-related problems. Screening patients for substance use/abuse, SDB and self-medication with OTCs will provide useful information when patients present with sleeping difficulties. The Epworth Sleepiness Scale (ESS) is a simple and efficient test to determine the degree of daytime sleepiness. Patients with a high ESS and a BMI >25 are at risk of sleep-disordered breathing2.
References
1. Bliwise DL (2004) Sleep disorders in Alzheimer’s disease and other dementias. Clin Cornerstone 6 Suppl 1A S16-28
2. British Snoring & Sleep Apnoea Association (2007) Patient Information. www.britishsnoring.co.uk
3. Brown D (2006) The effects of medication on sleep. Respiratory Care Clinics of North America 12 81-99
4. Cooke JR et al (2006) Acetylcholinesterase inhibitors and sleep architecture in patients with Alzheimer’s disease. Drugs & Aging 23 (6) 504-511
5. Cooke JR et al (2006) The effect of sleep disordered breathing on stages of sleep in patients with Alzheimer’s disease. Behav Sleep Med 4 (4) 219-27
6. DeMartinis NA & Winokur A (2007) Effects of psychiatric medications on sleep and sleep disorders. CNS & Neurological Disorders 6 17-29
7. Drapeau C et al (2006) Challenging sleep in aging: the effects of 200mg cafeine during the evening in young and middle-aged moderate caffeine consumers. Journal of Sleep Research 15 133-41
8. Gengo F (2006) Effects of Ibuprofen on sleep quality as measured using polysomnography and subjective measures in healthy adults. Clinical Therapeutics 28 (11) 1820-1826
9. Hudgel DW & Sitthep T (1998) Pharmacologic treatment of sleep disordered breathing. American Journal of Respiratory Care & Critical Care Medicine 158 (3) 691-699.
10. Johnson EO et al (1998) Epidemiology of alcohol and medication as aids to sleep in early adulthood. Sleep 21 (2) 178-186
11. Kosinski M et al (2007) Pain relief and pain related sleep disturbance with extended release Tramadol in patients with osteoarthritis. Current Medical Research & Opinions 23 (7) 1615-1626
12. Lam R (2006) Sleep disturbances and depression: a challenge for antidepressants. Int Clin Psychopharmacol 21 (suppl 1) S25-S29
13. Lu B et al (2005) Sedating medications and undiagnosed OSA: Physician determinants and patient consequences. J Clin Sleep Med 1 (4) 367-371
14. Onen H et al (2005) How pain and analgesics disturb sleep. Clin J Pain 21 (5) 422-431
15. Teplin D et al (2006) Screening for substance use patterns among patients referred for a variety of sleep complaints. The American Journal of Drug and Alcohol Abuse 32 111-120
16. Verster J et al (2004) Residual effects of sleep medication on driving ability. Sleep Medicine Reviews 8 309-325
17. Wilson S et al (2002) Effects of 5 weeks of administration of fluoxetine and dothiepin in normal volunteers on sleep, daytime sedation, psychomotor performance and mood. Journal of Psychopharmacology 16 (4) 321-331
18. Woods L & Craig T (2006) The importance of rhinitis on sleep, daytime somnolence, productivity and fatigue. Curr Opin Med 12 390-396
19. Zhang L et al (2006) Cigarette smoking and nocturnal sleep architecture. Am J Epidemiol 164 529-537