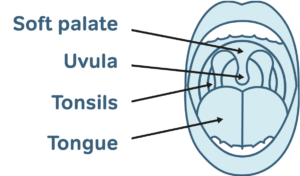
Radio-frequency ablation is designed to shrink redundant tissue of the soft palate. The treatment involves heating the inner tissue to 85ºC which results in the tissue beneath the skin being scarred. Somnoplasty is minimally invasive and creates controlled lesions that have little effect on surrounding tissues. The procedure takes about 20 minutes, can be performed in an outpatient clinic and does not carry the same complications as the other procedures. However, this is still a relatively new procedure and some surgeons prefer to perform the procedure under general anaesthetic. Somnoplasty generally requires the patient to undergo several treatment sessions but unlike the other procedures is much less painful. The applications of Somnoplasty are expanding and to date it is useful for turbinate and palate-based snoring.
Interestingly, one study reported that the chance of success from somnoplasty was considerably less in subjects with a Body Mass Index (BMI) in excess of 30, i.e., obese patients. Another study reported that 7 of 11 patients who underwent somnoplasty was dissatisfied with the procedure, stating that although there had been a moderate benefit it was not as good as expected.
In Germany, trials have recently been undertaken to reduce the tongue as a treatment for tongue-base snoring and obstructive sleep apnoea. Results however were not encouraging. These trials were conducted on a very small number of patients. Despite improvement in daytime sleepiness and subjective snoring levels after an average of 3.4 treatment sessions per patient, only 33% reported success.